What Lies Ahead? Vigilance and Hope
"[Preparations across Canada in anticipation of the new virus saw thousands of hospital beds including critical care beds with ventilators, freed in preparation for a feared flood of critically ill people infected with COVID; a mass casualty response] as if a hundred airplanes had crashed [simultaneously].""We understand now that within 24 to 48 hours, we can be responsive -- we proved that in March when we created capacity for a lot of patients. It can be reactive for local testing, and it can be regional.""We know better how to identify the disease and contact trace. We can't continue to function as we did in March, if there were a second wave."Dr.Jonathan Irish, cancer surgeon, Princess Margaret Cancer Centre, Toronto"The national epidemic curve could be highly variable, and while we are hoping for the 'snow burn' pattern, public health authorities are preparing for a potentially high fall peak [followed by other waves] that may exceed their current capacity to respond optimally."Public Health Agency of Canada"[Originally mixed messaging prevailed, a lack of clarity, a] desultory, lethargic and reactive and plodding response. Canada is low risk [was the mantra received from federal health officials. Except] we could see what was potentially coming and nothing was happening.""What's happened to the heart attacks [the strokes, the people with appendicitis-like pains? People were delaying seeking care] and we partly own that. We should have done a better job letting the public know our departments are safe, we've adapted, we're maintaining physical distancing and it's safe to come to the emergency department.""No hospital in this country has seen an occupancy rate of 85 percent in the last 20 years until this spring. If we allow that number to creep back up again, the resilience of our system is going to be impaired.""[Emergency rooms shouldn't be the nidus of hospital-acquired infections], and part of the thing we can do as emergency physicians is enhance things like virtual care, more effective telephone triage to prevent people having to crowd like herds of cattle in our waiting room for assessments.Our view has always been, look, better to be over-prepared than ill-prepared. If, with the passage of time and judgement of history, it's deemed we over-reacted, fine. I would far prefer that than to not have reacted appropriately at all. So we'll see." Dr.Alan Drummond, emergency physician, Canadian Association of Emergency Physicians
Dr. Irish and his colleagues expressed their frustration that it will take 84 weeks to clear the surgical backlog owing to COVID-19's entrance to Canada when all pending surgeries were cancelled during the emergency rush to prepare hospital beds for an assumed incoming of COVID-19 seriously ill patients. Their study was published in Canada's top medical journal where they estimated three-and-half months would be required to work through 'time-sensitive' cases such as cancers and coronary artery bypass grafts, and more than a year and a half to clear all pending surgeries inclusive of joint replacements and cataract and hernia repairs. In total, an estimated 148,364 surgeries.
"Obviously, the impact on our patients has been a profound one", commented Dr. Irish, added to the sheer magnitude of the surgical backlog. This, while Canada awaits the unknown but anticipated resurgence predicted to arrive in weeks and months of the second wave of COVID-19. Not that Dr.Irish feels the surgical hesitation and postponement of critical operations was not necessary in light of what little anyone really knew of the new virus outcomes. At the time what occurred was likely unavoidable in preparation of an unknown pandemic wreaking havoc the world over.
Now, however, doctors and hospital authorities understand that simply because one city realizes an increase in cases, the reaction should not be imposed on another city miles away which has experienced no such emergency. A plan is in the works to keep operating on people who are not ill with the virus, but who present with other critical illnesses, even while COVID rages in the background. Doctors are now more confident that they can handle the issues surrounding this once-in-a-century disease and that it is not a requisite that all other medical procedures be sacrificed for full attention to be given COVID.
Canada made all the sacrifices, all the changes, all the emergency measures to ensure it could handle an inrush of critically ill COVID-19 patients, and in the end, the onslaught failed to materialize. Those cases which did occur were readily handled, while hospital beds elsewhere were empty, and emergency rooms were quiet, no emergencies presented themselves, people suffering medical emergencies were fearful of contracting COVID with hospital exposure, and hoped their symptoms would subside on their own.
Dr.Theresa Tam, Canada's Chief Public Health Officer, speculates something might occur to the SARS-CoV-2 virus causing COVID-19, in that its behaviour is unlike influenza, no seasonal pattern has been observed so far, it continues circulating and it's possible the virus might evince "a certain type of acceleration under certain conditions", or conceivably that a mutation might alter it completely. There lies the uncertainty, its unpredictability, its presentation so unlike all previous viruses.
Italy Spain, France, Germany, India, Brazil, Argentina, Russia and South Korea all grapple with resurgencies, while areas of Northern England under stay-at-home instructions have all reacted to circumstances beyond their control. In France, President Macron made masking mandatory in outdoor spaces of Paris, responding to flare-ups. On an aside note, there is irony here in spades; in that France had previously outlawed the religion-based wearing of face coverings, or veils.
In the U.S. Dr.Anthony Fauci urged Americans to wear masks, distance, avoid crowds. And according to Mike Ryan of the World Health Organization; take the pressure off the virus and it will boomerang back. The approach of cold weather relates to increased indoor activities, with schools reopening and the appearance of seasonal flu. And hopes that whatever happens it can be managed, without seeing the horrors of health-impaired elderly people living in long-term care homes and retirement homes dying from COVID complications as a result of inexcusable unpreparedness.
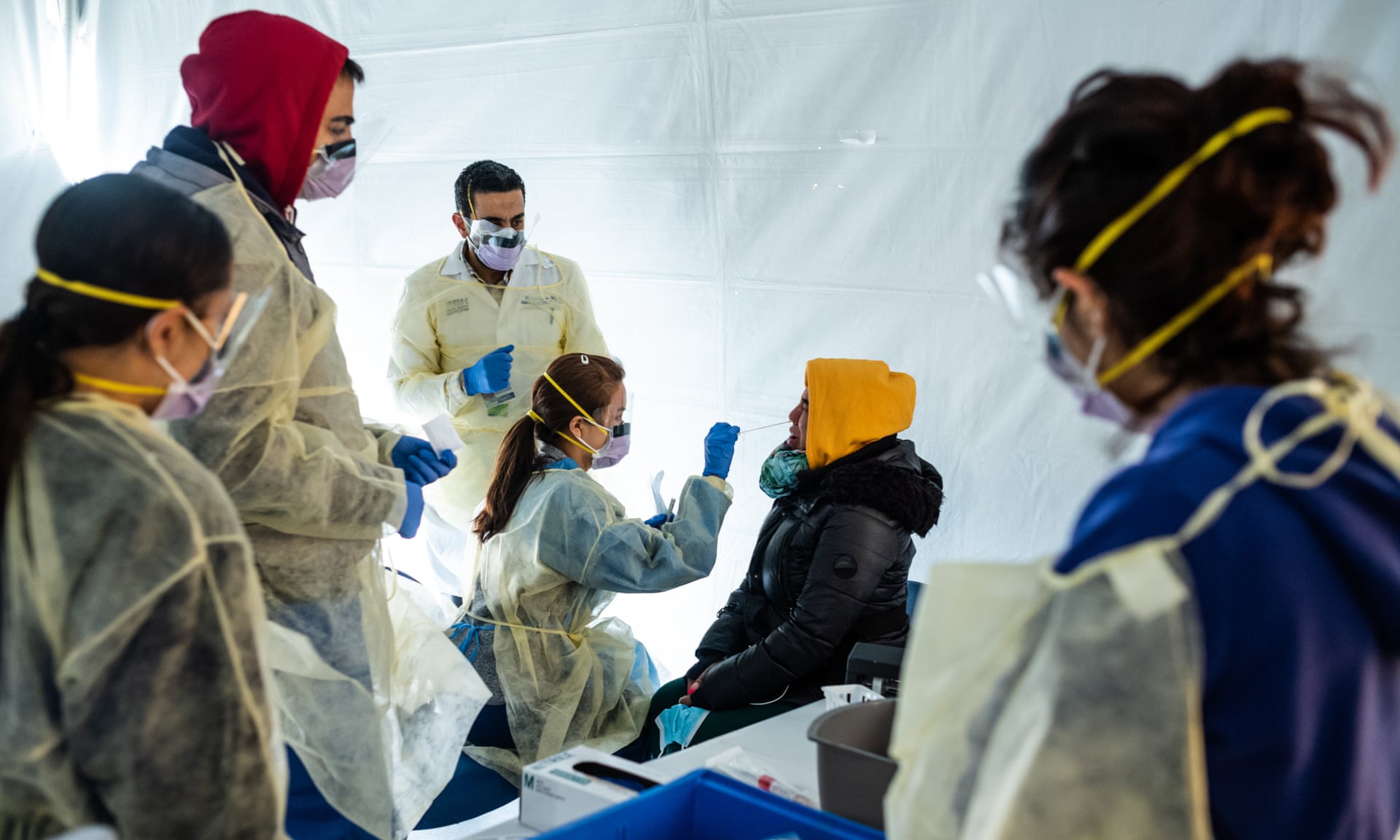 |
| It’s a completely new virus, so it’s really hard to know what would happen.’ Photograph: Misha Friedman/Getty Images |
In the final analysis the COVID-19 death rate in Canadian ICUs came out substantially beneath what was being seen in Italy or China. A flurry of studies gave additional evidence that common, inexpensive steroids are capable of cutting death rates in the most ill patients. There are any number of symptoms beyond fever, cough, shortness of breath, expanding to headache, loss of taste or smell, or inability to focus thoughts. Apart from which 20 to 40 percent of people have no or mild symptoms of the virus.
Over one percent of Canadians are thought to have antibodies to the virus while the vast majority has no immunity. A future of waste-water testing and pooled saliva testing allowing ten, 20, 30 people sampled in one test will facilitate an effort to become more efficient in analyzing and controlling the onset of disease. But how to account for people claiming COVID to be an elaborate hoax, a "clinical non-entity", among them some physicians espousing conspiracy theories...?

"[There has been a blip in sexually transmitted infections. Rising STIs tell us that] a certain segment of the population has abandoned all concepts of COVID precautions.""The problem is we cannot isolate young people from vulnerable people. It's just impossible to do that. Eventually, you lose out on the numbers game.""[Our surveillance system] is brutal. The one thing we should have learned but we haven't is that you can't rely on symptomatic testing alone to control an outbreak because there are just way too many people who don't have symptoms."Dr.Andrew Morris, infectious diseases physician"We don't have the magic bullet yet, but even with basic care, we're better. The single, solitary success story of the first wave was the effectiveness of public health measures -- travel restrictions, social distancing, mask-wearing. Enough people were compliant.""COVID is not a death sentence, by any stretch of the imagination."Dr.James Downar, specialist in critical and palliative care, University of Ottawa
 |
| Pedestrians wear masks as they walk in front of a sign reminding the public to take steps to stop the spread of coronavirus. (AP Photo/Chris Pizzello) |
Labels: Canada, Control, Novel Coronavirus, Second Wave
<< Home